SHOPP transition from fee-for-service to managed care presented
Posted on: 4/30/21
More than 150 OHA members tuned in for a SHOPP conversation presented by
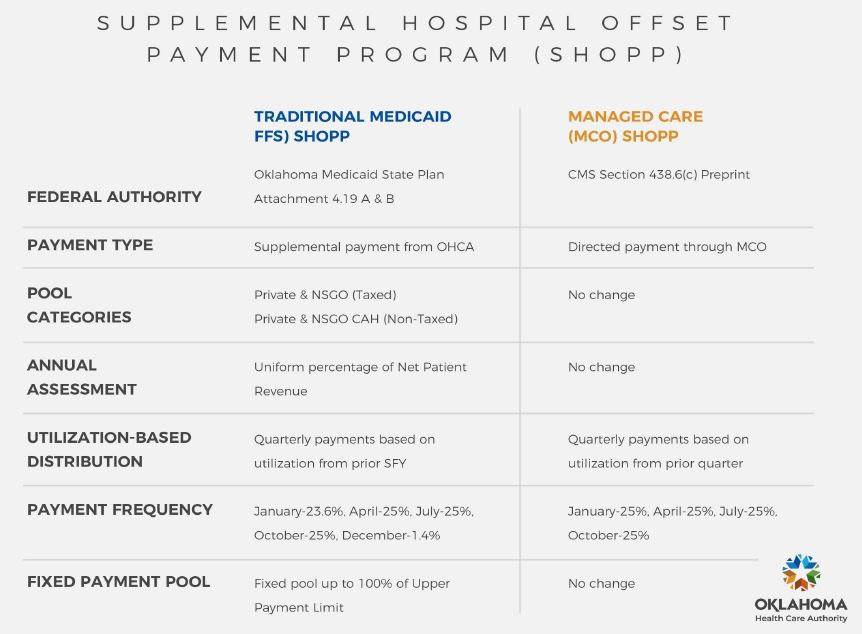
Aaron Morris, CFO, Oklahoma Health Care Authority on April 28. As proposed, hospitals will have both a SoonerCare SHOPP (current fee-for-service) for aged, blind, and disabled populations while pregnant women, children and the expansion population under the SoonerSelect managed care proposal would move to a directed payment program. OHA continues to oppose this proposal in the Legislature.
It is important to note: Under directed payments, for a hospital to receive the supplemental payment for each Medicaid patient encounter paid claim, the hospital
must be contracted with each MCO health plan. For patients who are out of network, the payment for hospital services would be limited to 95% of the existing Medicaid fee-for-service rate. Medicaid patients who do not choose an MCO plan will be auto assigned to a plan.
Below is a table that addresses the differences between the two programs.
The Medicaid MCO awards have been made to the following companies:
Medical Plans
BlueCrossBlueShield of Oklahoma
Humana Healthy
Oklahoma Complete Care (Centene)
United Healthcare
Dental Plans
DentaQuest
LIBERTY Dental
MCNA Dental
If the proposal is not defeated at the Legislature, the anticipated start of the proposal would be on Oct. 1. The Oklahoma Health Care Authority’s slide deck can be
found here and the recording of the meeting will be available soon on the OHCA website on the managed care page.
Morris also discussed SoonerCare Expansion (also known as Medicaid Expansion). The application process opens June 1, 2021, and coverage will begin July 1, 2021. Benefits under expansion will be the same as SoonerCare benefits today. OHA will be hosting an educational session on May 11 regarding the enrollment process.
(Mitzi McCullock)